Thursday, April 14, 2022
COVID-related Medicaid coverage extended – for now – for 500,000 Arizonans
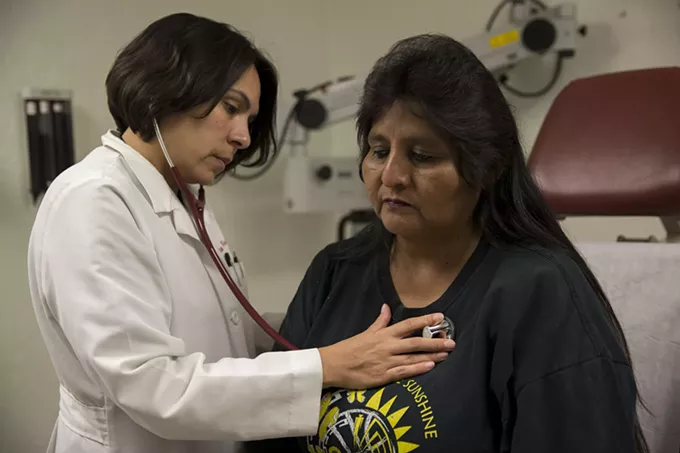
WASHINGTON – Federal officials threw a lifeline this week to as many as 500,000 Arizonans, just days before they were in danger of losing the Medicaid coverage they got under a COVID-19 public health emergency.
That emergency declaration, which was set to expire Saturday, was extended Tuesday for another 90 days by Health and Human Services Secretary Xavier Becerra.
Advocates welcomed the extension, but said it only delays the inevitable: When the emergency authorization eventually ends, the Arizona Health Care Cost Containment System will have to start weeding out some recipients.
“COVID has already shown us the vulnerabilities and the shortcomings of our system, which have been particularly painful for those who are the most underserved and vulnerable,” said Dr. Shad Fani Marvasti, director of Public Health, Prevention, and Health Promotion at the University of Arizona. “Disenrolling Medicaid is going to impact those folks in a really dire way.”
The decision to extend the public health emergency was unsurprising for many, since HHS had not given states the 60 days notice it has promised before lifting the authorization.
The HHS announcement came one day before the Centers for Disease Control and Prevention ordered a 15-day extension of its requirement that people be masked when traveling, which was set to expire Monday. The CDC said the move was needed so it could have time to study the impact of the latest COVID-19 variant, which has led to a slight uptick in cases this month.
The COVID-19 public health emergency was first declared in January 2020 and has been renewed nine times since, with the latest extension set to run through mid-July. As long as it is in effect, the state cannot remove people from the Medicaid rolls.
Under the Families First Coronavirus Response Act, signed into law March 2020, states get an additional 6.2% in federal funds to help pay for coverage of those enrollees while the public health emergency remains in place.
“AHCCCS has not disenrolled anyone from the program since March 2020,” said Heidi Capriotti, an AHCCCS spokesperson. Medicaid enrollment in Arizona increased by 26.7% since the start of the pandemic, covering 2.38 million residents as of this month.
But once the public health emergency ends, the state will be required to begin removing Medicaid recipients who no longer meet eligibility criteria. Capriotti said the state is preparing for that day, sending out letters to recipients to determine their eligibility, a task that is normally done monthly but has been suspended for the past two years.
AHCCCS estimates that about 500,000 recipients might need to confirm their eligibility to keep their coverage, which could lapse if the recipient got coverage from their work, aged into Medicare or makes too much money to qualify. Capriotti said recipients should make sure the state has the correct contact information to keep them from being dropped from the rolls because the state could not reach them.
“If we have their correct contact information and we can get a hold of them quickly, we can get ahead of the end date of this public health emergency,” Capriotti said. “But we don’t know when that’s going to happen.”
But health care advocates worry that the end of the public health emergency will not mean the end of the need for public health.
“There’s already too few resources available within the county system and too many people who need resources,” Marvasti said.
Zaida Dedolph, the director of health policy for the Children’s Action Alliance, said that lifting the emergency “does not necessarily mean that COVID is no longer a threat. But it means that things have sort of abated to the point where we no longer need access to these flexibilities.”
Others worry that people will be dropped from coverage accidentally by AHCCCS employees faced with “compressing 24 months worth of (Medicaid eligibility) redetermination into just several weeks,” said Will Humble, executive director for the Arizona Public Health Association.
Capriotti said the state does not currently plan to hire additional staff to handle the increased workload of sorting through all the eligibility redeterminations once the emergency ends.
Those dropped from the rolls will be able to apply for coverage during a special enrollment period. But advocates said that might not be an affordable option for all those who are disqualified, especially those whose income pushes them just above the threshold.
“We’ve seen the poverty level adjusted each year for cost of living, but we don’t necessarily see income eligibility adjusted for cost of living,” Dedolph said.
The potential loss of coverage for hundreds of thousands of Arizonans could also overwhelm emergency rooms, which will be the only option for those who will have “the lack of insurance and access to good primary care,” Marvasti said.
“Not only should we not be stopping the coverage, disenrolling people, I think we should actually be expanding Medicaid to make it universal for anyone and everyone who can’t afford private insurance,” he said.
For more stories from Cronkite News, visit cronkitenews.azpbs.org.